Optimal brain function starts with a healthy gut. Discover the latest scientific findings on the gut-brain axis, the microbiome, and how they affect mood, focus, and mental clarity. Learn how diet and proper care for your gut flora promote better mental health.
Take care of your gut and your brain will thank you! Find out how diet and probiotics affect mood, focus, and mental well-being.
Table of Contents
- Gut-Brain Axis: The Invisible Connection
- Gut Microbiome and Mental Health
- A Diet for a Healthy Gut and Brain
- Probiotics and Psychobiotics – Support for the Mind
- Symptoms of Gut Dysbiosis and Impact on Focus
- Ways to Improve Digestion and Mental Clarity
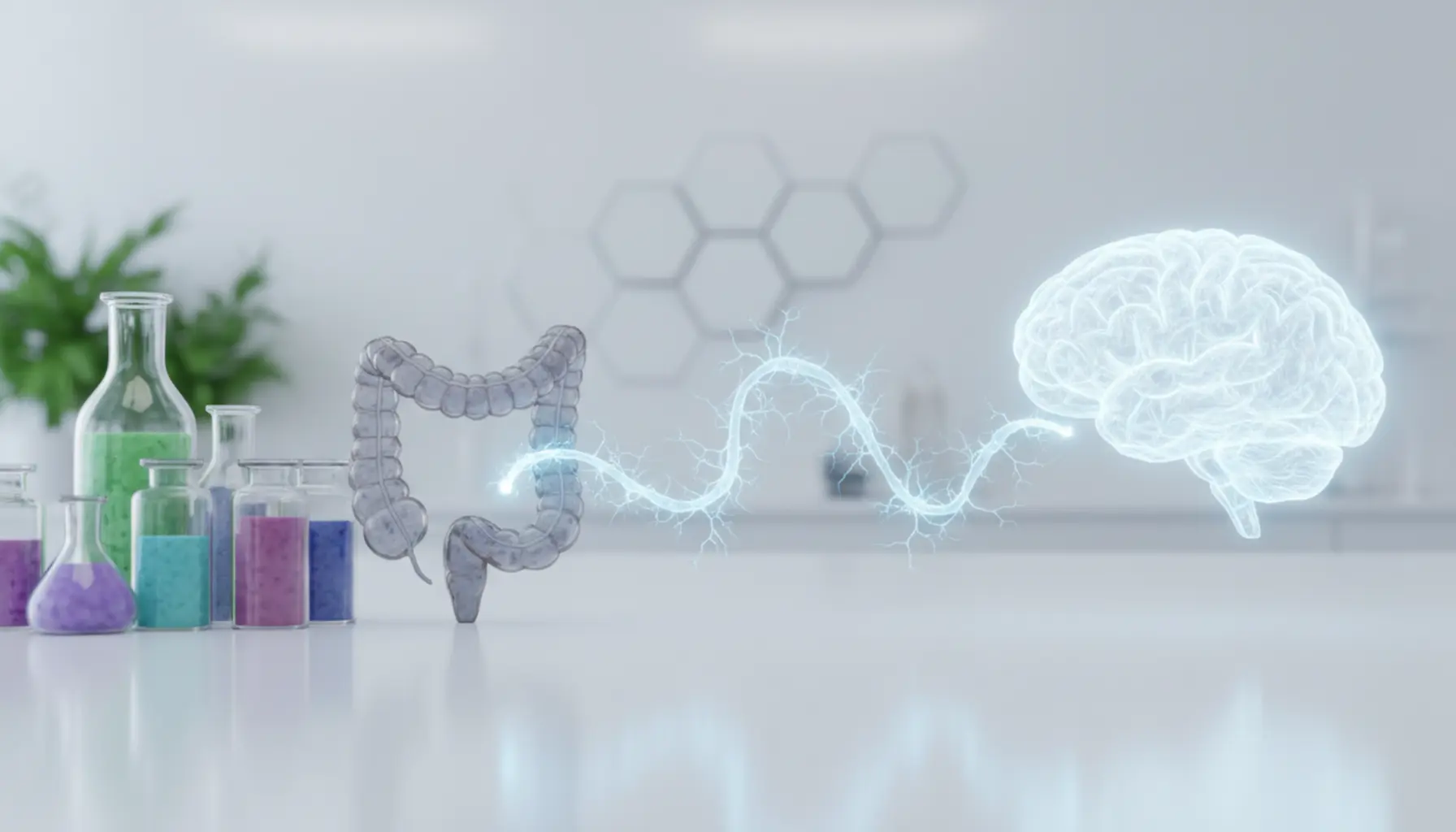
Gut-Brain Axis: The Invisible Connection
The gut–brain axis is a bidirectional communication system between the digestive tract and the central nervous system, operating constantly though often outside our awareness. Imagine it as a multi-lane highway where neural, hormonal, and immune signals travel in both directions. The brain regulates gut motility, enzyme secretion, appetite, and stress responses, while the gut and its resident bacteria send information back to the brain, influencing our mood, anxiety levels, concentration, and even how we respond to challenges. The vagus nerve, the longest cranial nerve running from the brainstem to the abdominal organs, plays a key role. Amazingly, up to 80–90% of the signals transmitted by the vagus nerve actually travel from the gut to the brain, not the reverse. This means the gut acts as a ‘control center’, constantly updating the brain about the body’s status: whether we’re satiated, if there’s inflammation, if stress hormones are high, or if energy levels are sufficient. This dialog can be ‘urgent’ (for example, sudden stomach pain during intense stress) or subtle and long-term, gradually influencing mental performance and well-being, or contributing to brain fog, irritability, and dips in mental energy.
While the vagus nerve is central to the gut–brain axis, the network is much more complex. The enteric nervous system (ENS), called the ‘second brain’, is involved with its network of about 100 million neurons in the gut wall, able to make autonomous decisions—regulating peristalsis, enzyme secretion, and responses to nutrients and toxins. The ENS stays in constant contact with the brain but often initiates and then reports on reactions. Another communication level involves hormones and neurotransmitters: up to 90% of serotonin (the ‘happiness hormone’) is produced in the gut. Gut serotonin mainly regulates gut motility, but its availability and metabolism indirectly affect mood and sleep cycles. Similarly, certain gut cells and the microbiota synthesize GABA and dopamine, creating a chemical ‘language’ for gut-brain communication. Cytokines and inflammatory mediators form the third channel: if the gut barrier is leaky, bacteria fragments and undigested food particles can enter circulation, stimulating the immune system and causing chronic, low-grade inflammation. This affects the brain—dampening focus, increasing fatigue, and in some individuals contributing to depression or anxiety symptoms. Thus, gut disorders like IBS, SIBO, or IBD often coexist with mental health problems, showing that the gut–brain axis is a real, physiological network with a direct impact on clear thinking and emotional stability.
Gut Microbiome and Mental Health
The gut microbiome—the community of trillions of bacteria, viruses, and fungi inhabiting our intestines—acts as an invisible biochemical lab, constantly communicating with the brain. Beyond digestion and immunity, gut flora influences mood, focus, anxiety levels, and even the risk of depression. Studies comparing the microbiome of healthy people with that of those experiencing mood disorders show clear differences in bacterial diversity and the presence of specific strains. People with depression often have a less diverse microbiome and a shortage of microbes that produce short-chain fatty acids (SCFAs) such as butyrate, propionate, and acetate. These substances not only nourish gut lining cells and strengthen the gut barrier but also influence brain function by regulating inflammation, neurotransmitter production, and gene expression related to stress response. In contrast, an excess of harmful bacteria (dysbiosis) can lead to toxin and pro-inflammatory metabolite production, resulting in more inflammation and disturbing neurological balance. Fascinating mouse experiments bred in a sterile environment (lacking microbes) revealed higher anxiety, worse stress resistance, and structural brain changes—normalized once beneficial bacteria colonized the gut. Similarly, gut flora disturbances in humans are associated with depression, anxiety, autism, or ADHD, and dietary or probiotic interventions are increasingly studied in psychiatric support.
The microbiome affects mental health via several pathways. First, gut bacteria modulate neurotransmitter production—some Lactobacillus and Bifidobacterium strains increase serotonin precursors (tryptophan), GABA, dopamine, and noradrenaline, key to mood, motivation, and pleasure regulation. Second, the microbiome makeup determines the level of pro- and anti-inflammatory substances; chronic, low-grade inflammation linked with dysbiosis and leaky gut is a recognized risk factor for depression and ‘brain fog’. Thirdly, bacteria influence stress hormone metabolism (e.g. cortisol) and stress-receptor sensitivity, influencing our response to daily challenges. People with a disturbed microbiome more often report irritability, sleep problems, difficulty focusing, and ongoing tension—even without obvious stressors.
An increasing body of evidence supports the existence of so-called psychobiotics—selected bacterial strains that benefit psychological function. Human studies show that certain probiotics can ease anxiety, improve mood, reduce perceived stress, and positively influence memory and processing speed. For example, Lactobacillus helveticus and Bifidobacterium longum combinations have been shown to lower cortisol and subjective stress in participants and improve sleep quality. Note that psychobiotic effects are strain-specific—not every ‘gut’ probiotic will be a ‘brain’ probiotic, so conscious, evidence-based selection is key. Environmental context also matters—the microbiome thrives on soluble fiber (from veggies, fruits, legumes, whole grains), fermented foods (sauerkraut, kefir, natural yogurt), healthy fats (olive oil, nuts, fatty fish), and dietary diversity. Conversely, diets low in fiber and high in sugar, processed foods, soda, fast food, and excess saturated fat favor dysbiosis and poor mental well-being. Chronic stress, sleep deprivation, excessive alcohol, smoking, and frequent unnecessary antibiotics also harm the microbiome. When this combination persists, gut signals to the brain increase tension, worsen mood, and impair cognition. Proactive microbiome care—through prebiotic diets, thoughtful probiotic use, stress management, and sleep hygiene—is foundational to preventing mood disorders and maintaining mental clarity. Psychological wellness isn’t just about therapy or medication—it’s also about your plate, your gut, and the microbes you invite to co-create your inner ecosystem.
A Diet for a Healthy Gut and Brain
A diet that supports both gut and brain isn’t based on one ‘magic’ food but on daily, repeated healthy choices. Diversity is key—the more varied, unprocessed plant foods you have daily, the richer and more stable your microbiome becomes. Dietary fiber, especially soluble fiber, acts as a (prebiotic) food source for beneficial bacteria. It’s found in fruits (apples, pears, berries), veggies (carrots, beets, artichokes, onions, leeks, garlic), legumes (chickpeas, lentils, beans), whole grains (oats, barley, rye), nuts, and seeds. Gut bacteria turn this fiber into short-chain fatty acids (SCFAs) like butyrate, propionate, and acetate, which reinforce the gut barrier, reduce inflammation, and support the brain. Regular intake of whole grains instead of white bread, pasta, or sugary breakfast cereals stabilizes blood sugar, providing a steady fuel supply for the brain and limiting mood swings and focus dips. Fermented foods are equally important, delivering natural cultures with probiotic properties. Traditional options include sauerkraut, pickled cucumbers, beet kvass, and dairy ferments like natural yogurt, kefir, and buttermilk (if lactose tolerance allows). Go for plain versions without added sugar or flavors, and prefer naturally fermented pickles (not vinegar-accelerated ones). Ideally, include small portions of fermented foods daily—e.g., a glass of kefir at breakfast or a few spoons of pickles at lunch—to consistently support gut microbial balance.
Fats, especially omega-3 fatty acids, are crucial for brain health, forming neural membranes, supporting anti-inflammatory processes, and potentially alleviating low mood. The best sources of EPA and DHA are fatty sea fish (salmon, herring, mackerel, sardines), eaten 2–3 times a week, as well as cod liver oil and quality fish or algae oil supplements (for plant-based diets). In everyday menus, replace saturated fats (red fatty meats, deli meats, fast food products) with healthy plant oils—extra virgin olive oil, cold-pressed canola, avocado, walnuts, almonds, flax, and chia seeds. This closely mirrors the Mediterranean diet, well-known for lowering depression risk and promoting healthy brain aging. Antioxidants also matter—compounds that neutralize free radicals which damage neurons and fuel inflammation. Colorful veggies and fruits are antioxidant-rich: berries, strawberries, cherries, pomegranates, kale, spinach, broccoli, peppers, beets, and tomatoes. Add a “rainbow” of colors to your daily meals for a simple brain shield against oxidative stress. The best gut-brain diet also minimizes sugar and ultra-processed foods. Excess sweets, soda, salty snacks, fast or ready-made meals cause glucose spikes, insulin resistance, increased inflammation, and microbiome impoverishment, potentially driving anxiety, irritability, and brain fog. Read ingredient lists, avoid foods full of additives and hydrogenated vegetable fats, and instead choose minimally processed fare: fresh produce, grains and brown rice, quality protein (fish, eggs, lean meat, legumes), nuts, and seeds. Supplements include gut and brain-boosting drinks: water as the primary beverage (dehydration decreases focus and causes headaches), modest amounts of green tea rich in calming L-theanine, and herbal teas (like lemon balm or chamomile) to relieve tension. Limit alcohol and excess caffeine—they harm the microbiome, disturb sleep, and dampen mood. Ultimately, treat this as a lifestyle, not a diet: gradually boost veggie portions, swap sweet snacks for fruit and nuts, introduce a weekly meatless day based on legumes, and ensure meal intervals are not too long to keep blood sugar, the microbiome, and your mind stable and clear every day.
Probiotics and Psychobiotics – Support for the Mind
Probiotics are usually associated with improved digestion, but their role goes far beyond curbing bloating or diarrhea. These live microorganisms, provided in adequate amounts, positively impact the host’s health—including brain function. More studies show that specific bacterial strains can reduce perceived stress, improve mood, and even support memory and concentration. When it comes to mental health impact, ‘psychobiotics’ come into play—probiotics (or their combinations with prebiotics) that reliably affect brain function and behavior. Their mechanisms are complex: gut microbes produce neuroactive substances (GABA, serotonin, dopamine), regulate pro- and anti-inflammatory cytokines, mediate stress responses via the HPA axis (hypothalamus–pituitary–adrenal), and affect gut barrier and blood-brain barrier permeability. When the gut is balanced, fewer toxins and inflammatory mediators enter the bloodstream, resulting in less brain ‘inflammatory noise’ and clearer thinking. That’s why targeted probiotic supplementation is increasingly investigated as a complement to therapy, medication, or lifestyle change.
Not every pharmacy probiotic is a psychobiotic; only carefully selected and clinically studied strains have demonstrated effects on the psyche—like reducing anxiety or bolstering stress resilience. Research frequently focuses on Lactobacillus and Bifidobacterium strains such as Lactobacillus rhamnosus, Lactobacillus helveticus, Lactobacillus plantarum, Bifidobacterium longum, and Bifidobacterium bifidum. Study participants taking these strains often report lower perceived stress, improved sleep quality, less irritability, and better cognition. Interestingly, these subjective results often parallel objective changes in markers: decreased cortisol, lowered inflammation, or altered brain region activity as seen on imaging scans. Psychobiotics aren’t ‘natural antidepressants’ or medication substitutes—they are one piece of the puzzle that can enhance the results of other mental health strategies. When choosing probiotics and psychobiotics, consider: first, the strain (identified by an alphanumeric code like Lactobacillus rhamnosus GG), as effectiveness is highly strain-specific; second, the dose expressed in CFUs (colony-forming units), with most studies using several to a dozen billion CFU daily; third, efficacy depends on supplementation time—usually a minimum of 4–8 weeks is needed to fairly evaluate effects on well-being and cognition. Also, effects are blunted if the diet lacks fiber, vegetables, and plant foods—bacteria need prebiotic ‘fuel’ to colonize the gut and make beneficial metabolites (SCFAs, B vitamins, anti-inflammatory compounds). Don’t forget natural daily probiotic sources: natural yogurt, kefir, buttermilk, sauerkraut, kimchi, pickles, or kombucha—regularly included, they enrich the gut ecosystem foundational to mood stability, stress resilience, and mental clarity. Combining probiotics with a supportive diet, stress reduction, sleep hygiene, and physical activity forms a synergistic approach to gut-brain care where microbes become partners in physical and mental well-being.
Symptoms of Gut Dysbiosis and Impact on Focus
Gut dysbiosis describes an imbalance between ‘good’ and ‘bad’ gut bacteria—triggered by low-fiber diets, chronic stress, antibiotics, or excess sugar and ultra-processed foods. While most people associate it with GI complaints, dysbiosis affects the brain powerfully. Classic digestive warning signs include bloating, gas, heaviness after meals, alternating diarrhoea and constipation, stomach pain, belching, a sense of incomplete evacuation, or ‘gurgling’ in the gut. Food intolerances often develop—foods previously well-tolerated start causing discomfort, rashes, headaches, or post-meal energy drops. Acid reflux, heartburn, or chronic nausea can also signal imbalanced flora. Many experience persistent fatigue and unexplained daytime sleepiness despite adequate nightly rest, often due to impaired nutrient absorption—gut microbes help synthesize and metabolize B vitamins, magnesium, iron, zinc, and fatty acids, all essential for neuron function. Deficiency directly reduces energy and focus. Symptoms also include skin problems (acne, eczema, hives), more frequent infections, reduced immunity, and weight fluctuations—unexplained gain or trouble putting on weight. Sugar and processed snack cravings often intensify—partly the ‘voice’ of harmful bacteria ‘demanding’ food to thrive. Mentally and emotionally, dysbiosis can manifest as irritability, outbursts of anger, baseless anxiety, low mood, or depression-like episodes. Unsurprisingly, people with IBS, SIBO, or chronic gut inflammation often report anxiety, insomnia, and psychological overload. Gut microbes generate substances affecting the nervous system—SCFAs, serotonin, GABA, dopamine—and disrupting their balance disturbs neurotransmitter regulation. A leaky gut barrier, common in dysbiosis, allows bacteria fragments and food particles into the bloodstream, fostering chronic low-grade inflammation. This weakens the blood-brain barrier, alters brain receptor sensitivity, and impairs neural signal transmission—causing ‘brain fog’: a hallmark yet frequently overlooked consequence of gut dysbiosis.
Brain fog is a subjective sense that ‘my mind isn’t working like it used to’—focus is harder, thought processes slow, short-term memory suffers, and simple tasks feel far more arduous. Gut microbiome imbalance can worsen fog in several ways. First: inflammation—pro-inflammatory cytokines penetrate the brain and alter the function of neurons tied to attention, planning, and decision-making. People with dysbiosis often report ‘energy crashes’ after eating, problems with logical thinking, inability to pull thoughts together, palpitations, anxiety, or mild derealization. Second: gut flora disruptions affect tryptophan metabolism—this amino acid’s proper processing is key for serotonin and melatonin production. If more tryptophan is diverted towards inflammatory pathways instead of serotonin synthesis, mood, sleep, motivation, and focus all decline. An overloaded, tired brain filters stimuli poorly and tires quickly. Third: dysbiosis disturbs the HPA axis (hypothalamus–pituitary–adrenal), vital to the body’s stress response. Overactivation chronically raises cortisol, further damaging gut lining and decreasing neuroplasticity—the brain’s capacity for new connections. This ‘stress–gut–brain’ connection means people under high occupational pressure, who sleep too little or eat on the go, often complain about distractibility, poor working memory, struggles with learning new info, and weak resistance to distractions. Dysbiosis can also deregulate blood sugar—unstable glucose brings energy crashes, mood swings, ‘mental emptiness’, and drives reliance on caffeine and sugar to ‘wake up’. Practically, someone with dysregulated gut flora struggles to keep their eyes on text, re-reads paragraphs, loses train of thought in conversation, forgets appointments or to-do lists, and feels easily overloaded by noise, multitasking, or open-plan offices. Look for cyclical symptoms—if your focus drops noticeably when gut issues (bloating, ‘tummy turmoil’, diarrhea or constipation) flare, and rebounds in ‘good’ periods, your microbiome likely plays a pivotal role. Of course, attention, memory, or mood problems can have many causes: hormone imbalances, neurological diseases, or chronic non-gut-related stress. But growing research on the gut–brain axis shows checking the microbiome for dysbiosis should be among the first steps when tackling persistent brain fog, poor intellectual performance, or everyday concentration difficulties.
Ways to Improve Digestion and Mental Clarity
Improving digestion and mental clarity begins with simple daily routines supporting the gut–brain axis on several levels. First is how you eat, not just what’s on your plate. Eating in a hurry, in front of computers or phones, activates the sympathetic ‘fight-or-flight’ system, inhibiting digestion. Practice mindful eating: take several steady breaths before meals, put away screens, focus on your food’s smell and taste, and chew every bite thoroughly. Good chewing eases the stomach’s workload, enhances nutrient use, and reduces bloating risk—yielding more stable energy and less post-meal brain fog. Meal regularity is critical. Big, heavy meals after long fasts overload digestion and cause glucose spikes, often experienced as a sudden burst of energy followed by a motivation slump, drowsiness, and irritability. For many, three main meals a day plus one healthy snack works best, eaten at roughly the same times. Hydration matters—water supports saliva, digestive juice, gut motility, and metabolic waste removal, including pro-inflammatory substances that affect mood and focus. Start your day with a glass of water, then drink consistently; avoid gulping large amounts at once. For healthy digestion and neurotransmitter balance, stabilize blood sugar: every meal should have protein (fish, eggs, legumes), healthy fat (olive oil, nuts, avocado), and fiber (veggies, whole grains). This slows glucose absorption, prolongs satiety, and delivers steady energy for the brain, aiding concentration and mood across the day. Also, reduce foods that fuel dysbiosis and inflammation: sodas, pastries with glucose-fructose syrup, fast foods, ultra-processed snacks, and trans fats. Many find that reducing these for a few weeks improves gut comfort, clarity of thought, and logical reasoning abilities. Helpful digestion ‘boosters’ include bitter vegetables (arugula, chicory, endive), spices (ginger, turmeric, fennel, caraway), and herbal teas (peppermint, chamomile, lemon balm)—stimulating digestive juices, reducing gut spasms, and supporting relaxation for quality mental rest. Sleep hygiene is crucial—sleep deprivation affects ghrelin and leptin (hunger and satiety hormones), increases sweet cravings, raises inflammation, and directly undermines the microbiome and cognitive function. Fixed bedtimes, less blue light in the evenings, and avoiding heavy meals 2–3 hours prior to sleep all boost both gut wellness and morning mental clarity.
As important as diet along the gut–brain axis is how we regulate stress and physical activity, since both directly shape the microbiome and inflammatory response. Chronic stress raises cortisol and adrenaline, altering gut permeability and microbiota, prompting symptoms like stomach pain, diarrhea/constipation, plus irritability, anxiety, and trouble focusing. Stress management practices—daily brief breathing exercises, mindfulness meditation, yoga, gentle stretching, or even 5–10 minutes of peaceful walking—activate the vagus nerve and ‘rest and digest’ mode, while improving the brain’s handling of sensory input. Physical activity is a powerful, simple ‘medicine’ for both gut and mind. Regular movement (brisk walks, cycling, swimming, dancing) increases microbial diversity, improves gut motility, supports neurogenesis and BDNF release—a brain fertilizer for memory and learning. It’s about consistency, not intensity—150 minutes of moderate activity per week is where many notice lower ‘heavy head’ symptoms, fewer post-meal crashes, and better mood. Don’t forget circadian rhythms: morning daylight and reduced artificial light in the evening stabilize the body clock, benefiting appetite, digestion, and mental alertness hormones. Another daily tactic: carefully track your body’s responses to specific foods. A symptom journal—logging what you eat and how you feel (physically, emotionally)—can reveal intolerances driving bloating, abdominal pain, and post-meal fog or mood swings. Sometimes you may need to cut certain food groups (e.g., high-FODMAPs) temporarily under professional supervision, giving the gut lining and microbiome a chance to recover. Many people also benefit from pre-meal relaxation rituals—deep breaths, brief work breaks, or a short gratitude practice shifting attention from stress triggers to the meal experience. This calms digestive–brain signals, enhancing nutrient utilization, neurotransmitter production, and fostering inner balance, improved focus, and greater daily mental clarity.
Summary
By caring for your gut health, you support not just digestion but also sharper mental function and emotional stability. The gut-brain axis shows how the gut microbiome impacts mood, focus, and clarity of thought. A proper fiber- and probiotic-rich diet effectively sustains microflora, reducing the risk of dysbiosis and mental health issues. Making fermented foods and relaxation a habit invests in mental clarity and lasting well-being. Your gut is your second brain—never forget it!